Learn More About Beta Blockers
Beta blockers are some of the most widely used medications in the world, prescribed for heart conditions, anxiety and more. Safe, easy to use and effective, they provide fast and noticeable results that make them ideal for preventing chronic anxiety and panic attacks.
Our guide to propranolol goes into more detail on how one of the most widely used beta blocker medications works, from its history to major benefits, potential side effects, drug interactions and more.
This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for and should never be relied upon for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment.
Get updates from hims
You May Like: Does Ibuprofen Make Asthma Worse
Can You Take Propranolol With Inhaler
propranolol albuterol Using propranolol together with albuterol may reduce the benefits of both medications, since they have opposing effects in the body. In addition, propranolol can sometimes cause narrowing of the airways, which may worsen your breathing problems or trigger severe asthmatic attacks.
How Might The Two Types Of Medicines Interact
In years past, experts were concerned that beta blocker medicines would interfere with how well beta agonists worked. They also feared that beta blockers would cause further constriction of already tight and narrow airway muscles in people with asthma. As a result, doctors were often reluctant to prescribe a beta blocker to a patient with asthma. Obviously, if the patient also had other health conditions that could benefit from a beta blocker, this could be problematic.
Fortunately, there have been many studies that have looked at beta blocker use in people with asthma.3 However most of these studies involved the use of cardioselective beta blockers. Researchers have found that this type of beta blocker presents very limited risk to people with asthma, as long as the recommended doses are followed. This is true even if the person with asthma is on a beta agonist.
Nonselective beta blockers have been found to decrease the response to beta agonists and should not be prescribed for people with asthma, if at all possible.3
Also Check: Is Asthma A Health Problem
Data Source And Population For Pharmacoepidemiological Studies
Data were extracted from the UK Clinical Practice Research Datalink which contains electronic medical record data from > 5 million UK people , , . People with medically treated asthma and ocular hypertension were identified by Read Codes and prescriptions for asthma and ocular hypertension medicines. The cohort consisted of people 18 years of age present in the CPRD between 1 January 2000 and 31 December 2011. Subjects were eligible if they: were permanently registered with a general practice for 1 year were from hospital episode statistics linked practices were defined by the CPRD as being acceptable for use in research had a Read Code for asthma and were issued one or more prescriptions for ocular hypertension medicines.
Medicines Can Trigger Asthma
Sometimes a medicine or supplement can trigger asthma symptoms. Be sure to tell your health care provider about all medicines, herbs, supplements and vitamins you take.
Make sure all the health care providers you see know you have asthma. Talk with your health care provider before starting any of the following:
- Aspirin
- Non-steroidal anti-inflammatory drugs, like ibuprofen and naproxen
- Beta-blockers, which are usually used for heart conditions, high blood pressure and migraines
For example: :
- Corgard®, nadolol
- Visken®, pindolol
- Trandate®, labetalol hydrochloride
ACE inhibitors, which are used for heart disease and high blood pressure, can cause a cough which could be mistaken for an asthma symptom.
For example: :
- Accupril®, quinapril
- Vasotec®, enalapril
- Zestril®, lisinopril
Never stop a medicine before talking with your health care provider. If you currently take any of these medicines, call your provider to discuss the medicine and your asthma.
Also Check: How To Use Black Seed For Asthma
What Is A Beta Agonist
Beta agonists are a type of medicine used to treat asthma .4 They are sometimes known as bronchodilators because they relax the airways. Like beta blockers, beta agonists act on the beta receptors in certain types of cells. Namely, they act on the beta receptors found in smooth muscle tissue. However, today’s beta agonists are designed to focus primarily on airway smooth muscle tissue, while minimizing the effects on smooth muscle found in the heart.5
Rather than interfering with the beta receptors, however, beta agonists enhance the action of certain enzymes that bind to the beta receptors. The result is relaxation of the lining of the airways. Overall, these are the benefits of using a beta agonist:6
- Minimize the required dose of inhaled steroids
The Benefits Of Taking Beta Blockers
Beta-blockers are primarily known to help the heart slow down in times of distress or lower the effects of adrenaline hormones, especially on those with heart problems. Aside from these, the drug also has some other health benefits. For instance, beta-blockers can protect the bones of the body by preventing the kidneys from eliminating calcium into the urine. The drug can also block stress hormones like adrenaline, which over time, can cause the thinning of the bones because of a deficiency of calcium. Also, beta-blockers are not the first line of defense against bone-thinning, stronger bones will be an extra benefit when taking the medication. Here are the other benefits of such medications:
Effectiveness. There is substantiated evidence which shows that taking beta-blockers after a heart attack can considerably lower the risk of a repeat attack that can lead to an early death. Also, the chances of living a better and longer life are much greater. Studies have also shown that various beta-blockers function better for various conditions.
Cost. This is good news for the millions of people who depend on beta-blockers. The drug is inexpensive and is available in low-priced generic pharmacies. The choice now depends on which beta-blocker a person needs. The choice will also consider the other medical and cardiovascular conditions as well as the side effects.
You May Like: Is Exercise Induced Asthma Real
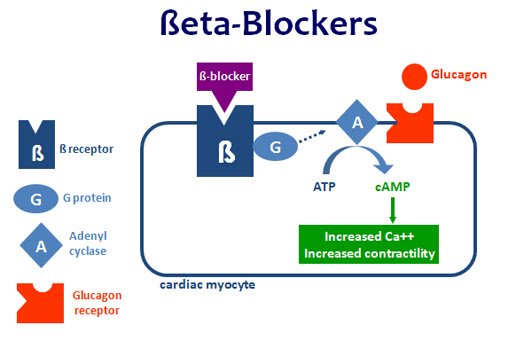
What Is A Beta Blocker
Beta blockers are a type of medicine developed in the 1960s that interfere with the body’s “fight or flight” response to stress.1 In response to stress or danger, your sympathetic nervous system releases adrenaline and noradrenaline. These are hormones that act as chemical messengers. Tiny proteins on the outer surface of many different types of cells called beta receptors sit and wait to latch on to these hormones. They then direct the body to respond in these ways:1,2
- The heart starts to beat faster
- Your blood vessels narrow and tighten
- The airways relax
- You sweat excessively
- Your blood pressure rises
All of those reactions can be useful in people who are in danger or who are responding to stress. But, in those with certain health conditions, such as angina or high blood pressure, those responses can be harmful. That’s where beta blocker medicines come in. They latch on to the beta receptors so that adrenaline and noradrenaline can’t bind to them.
As a result, this happens:2
- Your heart beats more slowly
- Electrical signals in the heart communicate better
- Your blood vessels throughout the body relax
- Blood pressure lowers
Do Not Suddenly Stop Taking Your Beta
Do not suddenly stop taking your beta-blocker without talking to your doctor first. This can be dangerous and make you feel unwell. You may get the feeling of changes in your heartbeat , an increase in blood pressure and a return of chest pains. If you do need to stop taking a beta-blocker then your doctor may advise a slow reduction in dose.
Dont Miss: Role Of Eosinophils In Allergy
Don’t Miss: How To Alleviate Asthma Cough
Why Shouldnt You Take Propranolol If You Have Asthma
Consequences. Despite safety concerns, propranolol is still prescribed to some people with asthma and anxiety. Propranolol exposure is associated with an increased risk of asthma hospitalization in susceptible individuals, which appears to vary with dose and duration of exposure.
Please enable JavaScript
What is the safest beta blocker?
A number of beta-blockers, including atenolol and metoprolol , have been designed to block only beta-1 receptors in heart cells. Since they do not affect beta-2 receptors in blood vessels and lungs, cardioselective beta-blockers are safer for people with lung disorders.
Beta Blockers: Are They Safe To Use If You Have Asthma
- Reactions 0 reactions
Traditionally, people with asthma who were on a type of medicine called a beta agonist were cautioned against using a type of heart medicine called a beta blocker. The concern was that these two types of medicine might interact in a way that was harmful to the patient. In this post, Ill give you the facts about both types of medicine and whether they truly do pose a risk when used together.
Don’t Miss: What To Do When You Get Asthma
The Relationships Between Beta
There are two types of beta-blockers, one can favor, and one can hinder the treatment of asthma and its medications
Beta-blockers are not manufactured equally or with the same properties.
As we mentioned above, there are two types of beta receptors as beta-1 and beta-2 receptors. Some beta-blockers are designed to be selective, only for the beta-1 receptors, to provide a more focused treatment.
This beta-blocker is called cardioselective beta-blockers. They only block the beta-1 receptors, the ones that stimulate the enzymes in the heart. In simple terms, cardioselective beta-blockers will only affect the heart functions.
The other beta-blocker is non-cardio selective, meaning they block both the beta-1 and beta-2 receptors. Blocking the receptors located in the lungs has a potential impact on asthma patients who experience breathing problems.
The lung receptors are responsible for relaxing the airways to make breathing easier. This creates the dilemma of using beta-blockers for patients with asthma and is a topic to be discussed with your doctor.
Beta Blockers Are Not Approved For Anxiety Reduction
Maybe the most important reason to avoid beta blockers is that theyâre not technically approved for anxiolytic use. Doctors prescribe these medicines âoff-labelââ meaning that they arenât approved for use but are used anyway.
Off-label use is not uncommon for medications â not even medications for anxiety. What makes beta-blockers unique is that not only are they used off-label but doctors arenât even sure why beta blockers reduce anxiety. Their mechanism is only partially known. Beta blockers lower heart rate and reduce norepinephrine, which can spike when a person has anxiety. This then controls the symptoms of anxiety. What is not entirely clear is whether or not beta blockers control any mental symptoms of anxiety. Doctors and patients sometimes find that people taking beta blockers seem to experience reduced anxiety, but it is not clear if any emotional symptoms are due to the beta blockers themselves, or just a reaction to weaker physical symptoms.
Recommended Reading: How To Increase Lung Capacity Asthma
What Do Beta Receptors Control
Beta receptors come in three different sub-types and have different functions depending on their location.
Beta-1
Beta-3
- Location: Fat cells and urinary bladder.
- What they do when activated:
- Cause fat cells to break down.
- Cause relaxation and increase in bladder capacity
- This also causes tremors, which limits potential medical applications for B3 receptor-targeted medications.
Risks Associated With Beta
People often worry taking a beta-blocker will make asthma or COPD worse. While selective beta-blockers are not as likely to cause pulmonary side effects as non-selective beta-blockers, they can cause pulmonary side effects, especially at high doses.
When taking these drugs, you may experience shortness of breath, wheezing, or more subtle respiratory effects that can be measured with diagnostic tests. Non-selective beta-blockers may lead to asthma or COPD exacerbations.
If you have asthma or COPD, your provider might suggest selective beta-blockers instead of non-selective beta-blockers. However, cardioselective beta-blockers have risks and side effects as well.
For example, they may reduce forced expiratory volume . This is more common when you first start taking them. FEV1 is a measure of the volume of air that you can expire with maximal effort in one second. In most cases, the FEV1 will normalize within a week or two once your body adapts to the drug.
Don’t Miss: Does Asthma Cause Lung Scarring
Beta Blockers Safe For Most Patients With Asthma Or Copd
Once upon a time in 1964, it was noted that propranolol, a nonselective beta-blocker, could precipitate severe bronchospasm in patients with asthma, especially at high doses. Additional small studies showed propranolol and other nonselective beta blockers could increase airway resistance. British guidelines advise avoiding beta blockers in asthma generally. As a result, beta blockers are often withheld from people with asthma or COPD who might benefit .
More recent evidence from multiple observational studies suggests newer, cardioselective beta blockers appear safe and might even be beneficial in people with COPD, potentially reducing mortality and exacerbations. However, in a randomized trial , patients taking beta-blockers had more-severe COPD exacerbations, on average.
Chronic use of beta blockers, including nonselective beta blockers like nadolol, may actually improve bronchodilator response to albuterol, through as-yet undetermined effects.
A very small randomized trial suggested that even nonselective beta blockers may be safer than previously believed for patients with mild to moderate asthma.
Whats more interesting is the question of whether chronic beta blocker use might actually improve asthma or COPD, as mounting observational evidence suggests. Enough safety data has accumulated that such prospective studies could be done ethically. There are a few small studies listed on clinicaltrials.gov testing beta blockers for asthma or COPD. Well keep you posted.
How Do They Work
Your body uses a chemical signaling system to control certain processes and functions. This uses specific sites on the surface of your cells, called receptors, where certain chemicals called neurotransmitters can latch on.
Receptors work similarly to locks. If a chemical with the right structure latches onto a receptor, it works like a key and activates the cell to respond a certain way. How the cell responds depends on where it is and what it does. If your body needs certain cells to act, it can produce more of the chemical that can activate the cells receptors.
Many medications work by artificially affecting that chemical signaling process. Medications that work like this fall into two categories:
- These medications attach to and activate receptor sites. In effect, they pretend to be the right kind of chemical compound and the cell falls for the deception. This can stimulate cells that wouldnt be active otherwise.
- These medications attach to the receptor sites but dont do anything else. The effect is similar to breaking a key after inserting it into a lock. The broken part of the key stays in place and blocks another key from entering. Antagonists reduce the number of receptors that are available for activation, which slows down cell activity.
Beta receptors
Beta blockers are beta receptor antagonists, meaning they block beta-adrenergic receptors and slow down certain types of cell activity.
Also Check: Does A Chest Xray Show Asthma
Beta Blocker In Asthma
- beta blockers are generally contraindicated in chronic obstructive airways disease and asthma
- note however that there is evidence that cardioselective beta blockers are > 20 times more selective for ß1 than ß2 receptors and should carry less risk of bronchoconstriction in reactive airways disease
- there is evidence that, in patients with COPD, cardioselective beta blockers do not change FEV1 or increase respiratory symptoms
- in a small study on asthmatics, propranolol caused a reduction in lung function, but celiprolol was shown not only to improve spirometry readings, it also inhibits the bronchoconstrictor effects of propranolol
- in mice studies, initial therapy with beta blockers increased airway hyperresponsiveness, whereas longer therapy decreased hyperresponsiveness and seemed to have an anti-inflammatory effect
Notes:
The Potential Risks Associated With Administration Of
In a double-blind, randomized, crossover study, Wilcox et al investigated the effect of metoprolol and bevantolol in 16 patients with asthma. Cumulative doses, ie, 12.5 mg, 25 mg, 50 mg, and 100 mg of metoprolol or 18.75 mg, 37.5 mg, 75 mg, and 150 mg of bevantolol, were administered at 2-hour intervals. Symptoms and lung function were monitored, and treatment was stopped if significant symptoms or a 20% decline in FEV1 were observed. The cumulative dosing regimen in general proved to be a safe and effective means of assessing bronchial responsiveness to -blockers in asthma, but one patient had to be withdrawn after the first dose due to severe bronchoconstriction. Of the 15 patients exposed to both -blockers, seven patients were withdrawn prematurely. The maximum tolerated cumulative dose of metoprolol and bevantolol was 26.8 mg and 45.5 mg, respectively, doses much lower than usually required for therapeutic activity. The authors concluded that even in patients who tolerate single doses of -blockers, the response to repeated treatment is unpredictable and, therefore, that -blocker therapy should be avoided in patients with asthma.
Recommended Reading: Does Smoking Weed Affect Asthma
