Treatment Of Exacerbations During Pregnancy
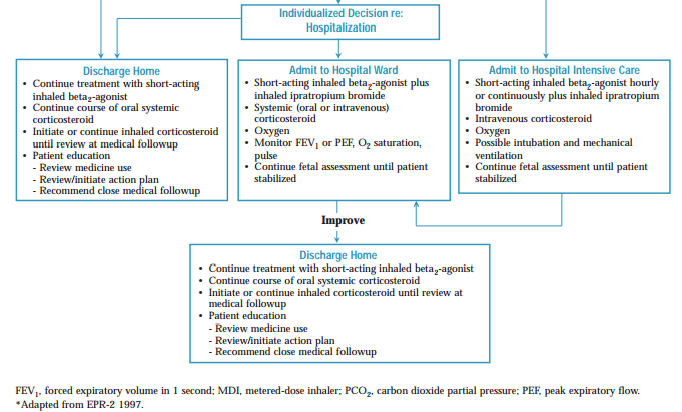
A study from the United States found that pregnant women presenting to the emergency department with an asthma exacerbation were significantly less likely to be given oral steroids either in the emergency department or on discharge from hospital than non-pregnant women. The pregnant women were also three times more likely than non-pregnant women to report an ongoing asthma exacerbation following discharge. It is important that treatment should be maximised during any asthma exacerbation which occurs during pregnancy. A severe asthma attack presents more of a risk to the fetus than the use of asthma medications due to the potential reduction in the oxygen supply to the fetus. In the event of an asthma emergency, women should receive close monitoring of lung function, oxygen saturation should be maintained above 95%, and fetal monitoring should be considered. In cases of severe asthma close cooperation between the respiratory specialist and obstetrician is essential.
Pregnancys Effects On Asthma
Asthma tends to follow the rule of thirds. Among pregnant women, one-third experience an improvement of symptoms, one-third experience a deterioration of symptoms, and one-third experience no change in symptoms.4 Factors that may improve the course of asthma during pregnancy include estrogen- or progesterone-mediated bronchodilation and descent of the fetus.5 Factors that may worsen the course of asthma include increased stress, gastroesophageal reflux, and increased occurrence of viral or bacterial respiratory tract infection.5
Multiple studies have demonstrated increased exacerbation and hospitalization rates in pregnant women with asthma.6-8 It is important to note that this increased incidence depends upon the severity of the asthma prior to pregnancy asthma.6 A classification of asthma severity and control appears in TABLE 1. Compared with pregnant women with mild asthma, those with severe asthma were more likely to experience a worsening of disease progression during their pregnancy.6 In a prospective, observational cohort study, pregnant patients classified as having mild asthma had an exacerbation rate of 12.6% and a hospitalization rate of 2.3% however, among pregnant patients with severe asthma, the exacerbation rate was 51.9% and the hospitalization rate was 26.9%.6
How Should I Prepare Before Pregnancy If I Have Asthma
Many healthcare providers recommend a preconception appointment before you start trying to get pregnant. This appointment is a chance to talk to your provider about any medical conditions you might have and your general health. Many people use this appointment to make a game plan for how they will want to treat their medical conditions like asthma during pregnancy. Its a chance to prepare with your provider for the upcoming pregnancy. Remember, you shouldnt stop taking any of your medications during pregnancy without first talking to your healthcare provider.
You May Like: Does Alcohol Make Asthma Worse
Is It Safe To Breastfeed
Doctors do not believe asthma medicines are harmful to a nursing baby when used in usual amounts. The transfer of asthma medicines into breast milk has not been fully studied.
When breastfeeding, drinking extra liquids to avoid dehydration is also important . Discuss this with your babys pediatrician.
Changes In Asthma Severity
![] Asthma Inhalers Used in Pregnancy Are Titrated to Asthma Severity ...](https://img.knowyourasthma.com/wp-content/uploads/asthma-inhalers-used-in-pregnancy-are-titrated-to-asthma-severity.jpeg)
About one-third of pregnant women with asthma will see their asthma symptoms get worse. Another third will stay the same. The last third will see their asthma symptoms improve.
Most women with asthma whose symptoms changed in any way during pregnancy will return to their pre-pregnancy condition within three months after giving birth.
If your asthma symptoms increase or decrease during one pregnancy, you may be likely to experience the same thing in later pregnancies. It is difficult to predict how asthma will change during pregnancy.
Because of this uncertainty, work with your doctors to follow your asthma closely. This way, any change can be promptly matched with an appropriate change in treatment. This calls for good teamwork between you, your obstetrician, your primary care physician, and your asthma specialist.
Read Also: How To Treat Asthma Wheezing
Treatment In The Emergency Department
Pregnant patients who present with typical mild exacerbations of asthma may be treated in the same way that a regular asthmatic patient with similar symptoms would be, with bronchodilator therapy and steroids.
Special attention must be given to pregnant patients who present with severe asthma exacerbations, because the resulting maternal hypoxia can have devastating consequences on the fetus.
The American College of Obstetricians and Gynecologists has issued practice guidelines for the management of asthma during pregnancy, Asthma in Pregnancy.
As always in the ED, address the ABCs. The patient should be placed on a cardiac monitor and pulse oximetry. The threshold of intubation should be low to prevent/limit hypoxic episodes to the fetus. Intubate and mechanically ventilate patients who are in or near respiratory arrest and patients who do not respond to treatment as evidenced by the following:
-
Hypoxemia despite supplemental oxygen
-
Persistent/worsening level of consciousness
-
Hemodynamic instability
The key to treating asthma in the pregnant patient is to frequently assess the patient, the severity of the attack, and the response to treatment.
Hypoxia, acidosis, unequal breath sounds, pneumothorax, and atypical features serve as warning signs of severe exacerbations.
The early use of systemic steroids has been shown to reduce the length of stay in the ED and the admission rate the effect of steroids is seen within 4-6 hours of the institution of therapy.
References
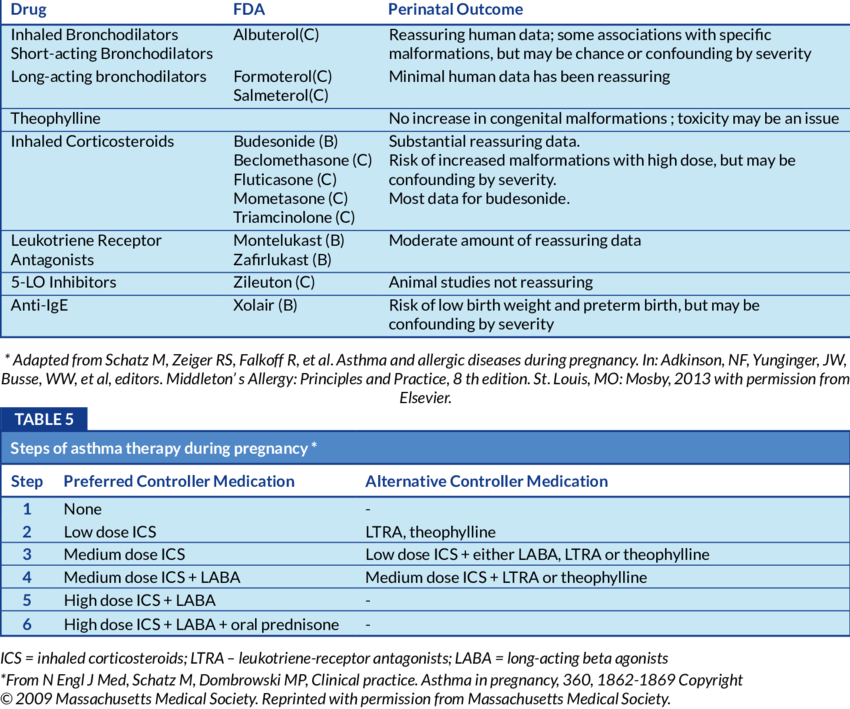
Asthma Treatment And Pregnancy
Pregnant women manage asthma the same way non-pregnant women do. Like all people with asthma, pregnant women should have an asthma action plan to help them control inflammation and prevent and control asthma attacks. Part of a pregnant woman’s action plan should also include recording fetal movements. You can do this by noting whether fetal kicks decrease over time. If you notice less fetal activity during an asthma attack, contact your doctor or emergency help immediately to get instructions.
Things to think about for asthma in pregnant women include the following:
Don’t Miss: Will Losing Weight Help My Asthma
Asthma And Pregnancy What To Expect
Because every pregnancy is unique, and everyones asthma is different, its hard to predict what will happen with your asthma when youre pregnant.
Some pregnant women find their asthma improves. Some don’t notice any changes in their symptoms at all. And some women especially those with severe asthma may find their symptoms get worse.
If you do notice changes in your asthma during pregnancy, these may not carry on once your baby is born. In most cases asthma goes back to how it was before you were pregnant.
If you have difficult or severe asthma ask your GP or asthma nurse if you need an asthma specialist to support you during your pregnancy. Its important to keep an eye on your symptoms, and make sure the medicines youre taking are working well.
Some women notice asthma symptoms for the first time during pregnancy
If this happens to you it probably means you had mild asthma without realising it. And pregnancy hormones in pregnancy have triggered your symptoms.
Exacerbations Of Asthma During Pregnancy And The Risk Of Low Birth Weight
Using data from three studies, there was a significantly increased risk for low birth weight in women who had an asthma exacerbation during pregnancy 2.54, 95% confidence interval 1.52 to 4.25) compared with women without asthma . There was no increased risk for low birth weight in asthmatic women who did not have an exacerbation during pregnancy compared with women without asthma. The difference between the relative risks of the exacerbation and no exacerbation subgroups was also significant 2.27, 95% CI 1.29 to 3.97).
Figure 1
Meta-analysis examining the risk of low birth weight infants from asthmatic and non-asthmatic pregnancies. Studies are grouped based on whether women had an exacerbation during pregnancy or no exacerbation of asthma during pregnancy. The relative risks with 95% confidence intervals are given.
Also Check: Pulmonologist Or Allergist For Asthma
You’ve Saved This Page
Asthma is a lung disease that causes your airways to tighten up, making it hard for you to breathe. Theres no cure for asthma. Even if you have asthma and feel healthy, asthma flares can happen at any time.
Most people with asthma can keep the disease under control and avoid serious health problems. If youre pregnant, its really important to work with your health care provider to manage your asthma and get medical care, if needed.
Etiologic Factors In Asthma
Asthma results from a complex and poorly defined interaction of genetic predisposition and environmental stimulation. The basic mechanism for nonspecific bronchial hyperresponsiveness is unknown. Airway inflammation is the most popular hypothesis.
Implicated stimuli include the following:
-
Allergens, including pollens, house-dust mites, cockroach antigen, animal dander, molds, and Hymenoptera stings
-
Irritants, including cigarette smoke, wood smoke, air pollution, strong odors, occupational dust, and chemicals
-
Medical conditions, including viral upper respiratory tract infections, sinusitis, esophageal reflux, and Ascaris infestations
-
Drugs and chemicals, including aspirin, nonsteroidal anti-inflammatory drugs, beta blockers, radiocontrast media, and sulfites
Also Check: Does Secondhand Marijuana Smoke Affect Asthma
Association Between Asthma Exacerbations And Adverse Perinatal Outcomes
There have been conflicting data on the association between asthma exacerbations and adverse pregnancy or fetal outcomes .
Table 2
Summary of studies investigating the association between asthma exacerbations and perinatal outcomes
Several studies have found that exacerbations of asthma during pregnancy are associated with low birth weight, pre-eclampsia, and perinatal mortality. However, other well designed prospective cohort studies have found no significant relationships between asthma exacerbations during pregnancy and poor perinatal outcomes, including preterm delivery, pre-eclampsia and low birth weight, in women with actively managed asthma.
Exacerbations Of Asthma During Pregnancy And The Risk Of Preterm Delivery
Using data from four studies, there was no significantly increased risk of preterm delivery in women who had an exacerbation of asthma during pregnancy or in women who did not have an asthma exacerbation during pregnancy compared with women without asthma . There was no difference between the relative risks for the subgroups with or without exacerbations .
Figure 2
Meta-analysis examining the risk of preterm delivery from asthmatic and non-asthmatic pregnancies. Studies are grouped according to whether women had or did not have an exacerbation of asthma during pregnancy. The relative risks with 95% confidence intervals are given.
Also Check: Does Asthma Increase Blood Pressure
Take Action If Your Asthma Symptoms Get Worse During Pregnancy
The sooner you get help the quicker you can cut the risks to you and your baby. So talk to your GP, asthma nurse, midwife, or pharmacist if you notice any of the following:
- Youre coughing or wheezing more especially at night.
- Your chest feels tight
- Youre taking your reliever inhaler more often. If youre taking your reliever inhaler three or more times a week, you may be at risk of an asthma attack and should get an urgent GP appointment.
- Your nose feels stuffy This is a common pregnancy symptom. But it could also affect your asthma. If your nose is stuffy youre more likely to breathe through your mouth instead. This means the air doesnt get warmed up before it hits your airways. And allergens cant be filtered out as well.
- You feel more breathless. Getting a bit breathless more than usual is another common pregnancy symptom. But dont ignore it. Its also a sign your asthma is getting worse.
- Your hay fever gets worse. Hay fever or pollen allergy can make your asthma symptoms worse so its important to treat it. Ask your GP or pharmacist about which hay fever treatments are safe for you to use during your pregnancy. Its likely that youll be recommended eye drops or nasal sprays first. You can also try other ways to relieve hay fever symptoms.
- You have acid reflux this is common in pregnancy and can make your asthma worse.
What to do if youre having an asthma attack
What You Need To Know
Many women find their asthma changes during pregnancy. Whether your asthma is better or worse, good asthma control when you are pregnant is vital for the best possible health for you and your baby.
Do not stop taking your asthma medications.
Stopping your medications can put your baby at risk.
Because you are breathing for your baby too, well controlled asthma means your baby will have a good oxygen supply for normal growth and development, preventing low birth weight and premature delivery.
Read Also: Is Montelukast Good For Asthma
Can Asthma Symptoms Change During Pregnancy
Yes, asthma symptoms often change during pregnancy. Sometimes they get better and sometimes they get worse. We dont really understand what causes these changes.
Getting the flu can set off serious asthma symptoms. Be sure to get a flu shot in October or November every year.
Heartburn also can make your symptoms worse. Heres what you can do to help with heartburn symptoms:
- Sleep with your head up on a pillow .
- Eat smaller meals several times a day.
- Dont eat within 2 hours of bedtime.
- Ask your provider about medicines you can take.
Do You Need Any Special Tests If You’re Pregnant And Have Asthma
If your asthma is under control and mild, you may not need any special tests. If your asthma is not well controlled or if your asthma is moderate to severe, your provider may recommend repeated ultrasounds to check to make sure your babys growing normally. Ultrasound uses sound waves and a computer screen to show a picture of your baby inside the womb. Your provider may start these at around 32 weeks of pregnancy.
Your provider also may recommend taking your babys heart rate with a fetal heart monitor. This allows him to check on your babys well-being.
Test results can alert your provider if you or your baby needs special care.
Don’t Miss: How To Run With Asthma In Cold Weather
Experiences Of Pregnant Women In Relation To Asthma Management In Pregnancy
Two studies have examined the perspective of pregnant women in relation to their asthma and asthma care during pregnancy. Limet al. conducted qualitative interviews with 23 pregnant women with asthma in Australia, at various stages of their pregnancy or up to 5weeks post partum. Some women expressed the view that there were risks associated with asthma medication use during pregnancy, particularly related to steroid use, and they were therefore cautious about using ICS unless desperate. Their views about the safety of reliever medication such as salbutamol were quite different, however, with women preferring to use a lot of reliever therapy rather than preventers. There were also women who were more concerned about the possible risks of uncontrolled asthma and whether the baby was receiving enough oxygen. In terms of management by health professionals, the women noted that their GP was not concerned about their asthma and that other issues with the pregnancy often took priority. In addition, there was a view that there was a lack of information given about asthma during pregnancy, and that doctors and pharmacists were unclear about the safety of medication use in pregnancy, forcing some women to make a decision for themselves or consult Dr Google, where they obtained unreliable or inaccurate information .
Antenatal Care For Uncomplicated Pregnancies
Asthma is the most prevalent chronic disease in pregnancy, and as symptoms can change with pregnancy, and exacerbations of asthma are common, regular review of asthma symptoms, the provision of self-management education, and appropriate medication use are the hallmarks of management. Co-morbidities are also prevalent among pregnant women with asthma, with obesity, gestational diabetes, hypertension, rhinitis, depression, and anxiety, more common among women with asthma than women without asthma. Less is known about reflux, obstructive sleep apnoea and vocal cord dysfunction, along with nutritional deficiencies to iron and vitamin D. Maternal asthma impacts the offspring’s long-term health, particularly in increasing the risk of early life wheeze and asthma in childhood. While breastfeeding may modify the risk of infant wheeze, less is known about the mechanisms involved. More research is needed to further understand the relationship between asthma in pregnancy and the risk of poor neurodevelopmental outcomes, such as autism.
Also Check: How Does Asthma Affect The Kidneys
Risks Of Uncontrolled Asthma To Pregnant Women
If you have not previously had asthma, you may not think that shortness of breath or wheezing during your pregnancy is asthma. If you know you have asthma, you may not consider it a concern if you only have mild symptoms. But asthma can affect you and your fetus, and you should act accordingly.
If your asthma is not controlled, risks to your health include:footnote 1, footnote 2
Risks to the fetus include:footnote 1, footnote 2
- Death immediately before or after birth .
- Abnormally slow growth of the fetus . When born, the baby appears small.
- Birth before the 37th week of pregnancy .
- Low birth weight.
The more control you have over your asthma, the less risk there is.
Acute Exacerbations Require Aggressive Management
Based on a systematic review, 20% of pregnant women with asthma require some intervention for an asthma exacerbation during pregnancy, and 5.8% are admitted to the hospital for an exacerbation. Exacerbations were associated with a higher risk of low birth weight compared with rates in women without asthma.
Exacerbations are more common late in the second trimester and are unlikely to occur during labor and delivery. The incidence of exacerbations increases with the severity of asthma, from 8% in mild asthma, to 47% in moderate asthma, to 65% in severe asthma. Risk factors for exacerbations include poor prenatal care, obesity, and lack of appropriate treatment with inhaled corticosteroids. The main triggers are viral respiratory infections and noncompliance with inhaled corticosteroid therapy.
Asthma exacerbations during pregnancy should be managed aggressively , as the risk to the fetus of hypoxia far outweighs any risk from asthma medications. Close collaboration between the primary care physician and the obstetrician allows closer monitoring of mother and fetus.
Read Also: Does Asthma Make You Cough Constantly
