Responsiveness To Inhaled Corticosteroids
There is a general feeling that patients with ACOS compared with patients with COPD are more responsive to inhaled corticosteroids. However, strong evidence is not available to support this notion. In one study, Parket al. evaluated FEV1 improvement after 3months of treatment with a fixed-dose inhaled corticosteroid/long-acting 2 combination . They found that patients with ACOS features were twice as likely than patients with COPD to have a significant therapeutic response to ICS/LABA. These results require validation and refinement before they can be adopted into clinical practice for patients with ACOS. For instance, it is not entirely clear that a 3month improvement in FEV1 with ICS/LABA will translate into improvements in patient-oriented or long-term outcomes and, in future studies, it may be more appropriate to evaluate ICS alone to clearly understand the impact of ICS therapy on ACOS patients.
Recommendation on ICS responsiveness in ACOS
How Is Acos Diagnosed
ACOS means you have symptoms of both asthma and COPD. Your doctor may diagnose asthma, COPD, or ACOS.
ACOS is a fairly new term. Exact guidelines for diagnosing ACOS havent been established. ACOS generally involves these three features compared with people who have COPD alone:
- more of a response to inhaled bronchodilators
- increased reversibility of airflow
- bronchial and systemic inflammation from eosinophils, a type of white blood cell
To reach a diagnosis, your doctor will perform a physical examination and review your clinical history. Imaging tests such as X-ray, CT scans, or MRI may be necessary. Its likely youll also need a noninvasive test called spirometry, also known as a pulmonary function test, to measure your lung function.
Because asthma causes inflammation, youll still need asthma treatment. This may include:
- allergen avoidance
- long-acting bronchodilators
- preventive vaccines, such as flu, pneumonia, and whooping cough
Youll also need to manage symptoms of COPD to maintain lung function. This may involve:
- disease management training
- avoiding smoke and other pollutants
- healthy eating and nutrition education
- long-acting bronchodilator combinations or combination bronchodilator or inhaled corticosteroids
- preventive vaccines, such as flu, pneumonia, and whooping cough
- oxygen therapy
- surgery to remove damaged lung tissue or air sacs
- doctors
Here are some other tips for managing ACOS:
Referral For Specialized Investigations
Referral for expert advice and further diagnostic evaluation is necessary in the following contexts : Patients with persistent symptoms and/or exacerbations despite treatment diagnostic uncertainty, especially if an alternative diagnosis including suspected pulmonary hypertension, cardiovascular disease, and other causes of respiratory symptoms, needs to be excluded patients with suspected asthma or COPD with atypical or additional symptoms or signs suggest an additional pulmonary diagnosis when chronic airways disease is suspected but syndromic features of both asthma and COPD are few comorbidities present referral may be appropriate for issues arising during ongoing management of asthma, COPD, or ACOS, as outlined in the GINA and GOLD strategy reports.2, 4
Guidelines of Global Initiative for Asthma and Global Initiative for Chronic Obstructive Lung Disease showed syndromic approach to disease of chronic airflow limitation. This approach showed from diagnosis of chronic airway disease to referral for specialized investigations
In summary, when diagnosis is uncertain or symptoms are atypical or continue in spite of appropriate treatment of ACOS by guidelines recommendations, referral for specialized investigation is needed.
You May Like: Are Oil Diffusers Bad For Asthma
Is It Asthma Copd Or Both
Both asthma and chronic obstructive pulmonary disease , including emphysema and chronic bronchitis, make breathing difficult. In fact, they share many similarities. However, they are different lung diseases. Asthma-COPD overlap syndrome is diagnosed when you have symptoms of both asthma and COPD. ACOS is not a separate disease, but rather a way for doctors to recognize the mix of symptoms and select a treatment plan that is most appropriate for you.
Implications Of Overlapping Asthma And Copd
How-to videos available from the National Asthma Council AustraliaPatients with coexisting asthma and COPD have an increased illness burden1 compared to those with asthma or COPD alone. They have more frequent and severe exacerbations9 and hospitalisations. This is despite having had fewer pack-years of smoking than those with COPD alone.9 Mortality may also be increased.1,10
Asthma may also be a risk factor for developing COPD.1,4,11 In severe asthma, structural changes such as airway remodelling can contribute to fixed airway obstruction and smaller airway size. Single nucleotide polymorphisms have been identified in biologically plausible genes associated with asthmaCOPD overlap but their significance is unclear.9
Don’t Miss: How To Avoid Asthma At Night
Genetics And Epigenetics Of Aco
|
Table 4 Different Single Nucleotide Polymorphisms Identified in Patients with ACO |
Hansel et al49 examined another potential definition of ACO by evaluating the genetic architecture of airway hyperresponsiveness of COPD patients in the Lung Health Study . They genotyped 2814 non-Hispanic whites and related the underlying genetic structure of these participants with their level of airway responsiveness at baseline and then at year 5 of follow-up. Although no SNPs reached the genetic threshold for statistical significance, 4 loci were identified that demonstrated nominal statistical significance . None replicated and only 2 of the genes near these SNPs were lung expression quantitative trait loci .
Another phenotype of ACO is responsiveness to inhaled corticosteroids. This was examined in Lung Health Study-2, which was a randomized controlled trial to evaluate the therapeutic benefits of inhaled corticosteroids on the rate of FEV1 decline over 3 years in approximately 800 patients with COPD. Obeidat et al50 did not find any SNPs that reached genome-wide significance. However, there were 2 SNPs that significantly modified the effects of ICS on the rate of FEV1 decline, which were replicated in an external cohort, the Advair Biomarker in COPD trial, which was a short-term randomized controlled trial that evaluated the effects of ICS on lung function in COPD patients.
Clinical Manifestations Of Aco
Studies that have reported on the clinical manifestations of ACO have focused on symptoms , health-related quality of life, lung function, exercise intolerance, and exacerbations which are considered most relevant to patients and to physicians.
Most studies reported that ACO results in more severe symptoms than asthma or COPD alone, including a recent study that observed a higher disease burden for eosinophilic ACO compared with eosinophilic COPD or asthma.30 However, several individual trials and a systematic review suggested that this affirmation should be nuanced.31 Indeed, looking at each manifestation individually provides a better overview of the impact of ACO on patients. In terms of symptoms, it appears that patients with ACO experience more wheezing and mucus production than patients with asthma or COPD.32,33 Higher Medical Research Council scores suggest that ACO patients also have more dyspnea24,25,27 with the three populations: asthma, COPD and ACO, otherwise being quite similar regarding symptoms.
In conclusion, despite the differences in diagnostic criteria for ACO, the majority of studies have reported a high symptom burden associated with ACO, with a significantly higher frequency and severity of exacerbations compared with asthma and COPD.
Recommended Reading: Can You Have Asthma And Copd
Bronchodilator Treatment In Asthma And Copd
There are 2 major classes of inhaled bronchodilators: 2-agonists and anticholinergic agents within each of these classes, both short-acting and long-acting formulations are available. The presence of acute reversibility with the use of bronchodilators does not completely distinguish asthma from COPD. Patients with either condition can benefit from bronchodilators and should be given a trial to assess their response. Furthermore, bronchodilators have been consistently shown to induce long-term improvements in symptoms, exercise capacity, and airflow obstruction in patients with COPD, even when there is no spirometric improvement after a single test dose.,
The bronchodilator responses in asthma and COPD differ both quantitatively and in their spirometric patterns. While asthmatic patients typically show an increase in FEV1 alone or in both FEV1 and forced vital capacity , patients with COPD typically display an isolated increase in FVC or in both FEV1 and FVC .,
Bronchodilators in the Treatment of Acute Exacerbations of Asthma and COPD
Bronchodilators in the Treatment of Stable Asthma and COPD
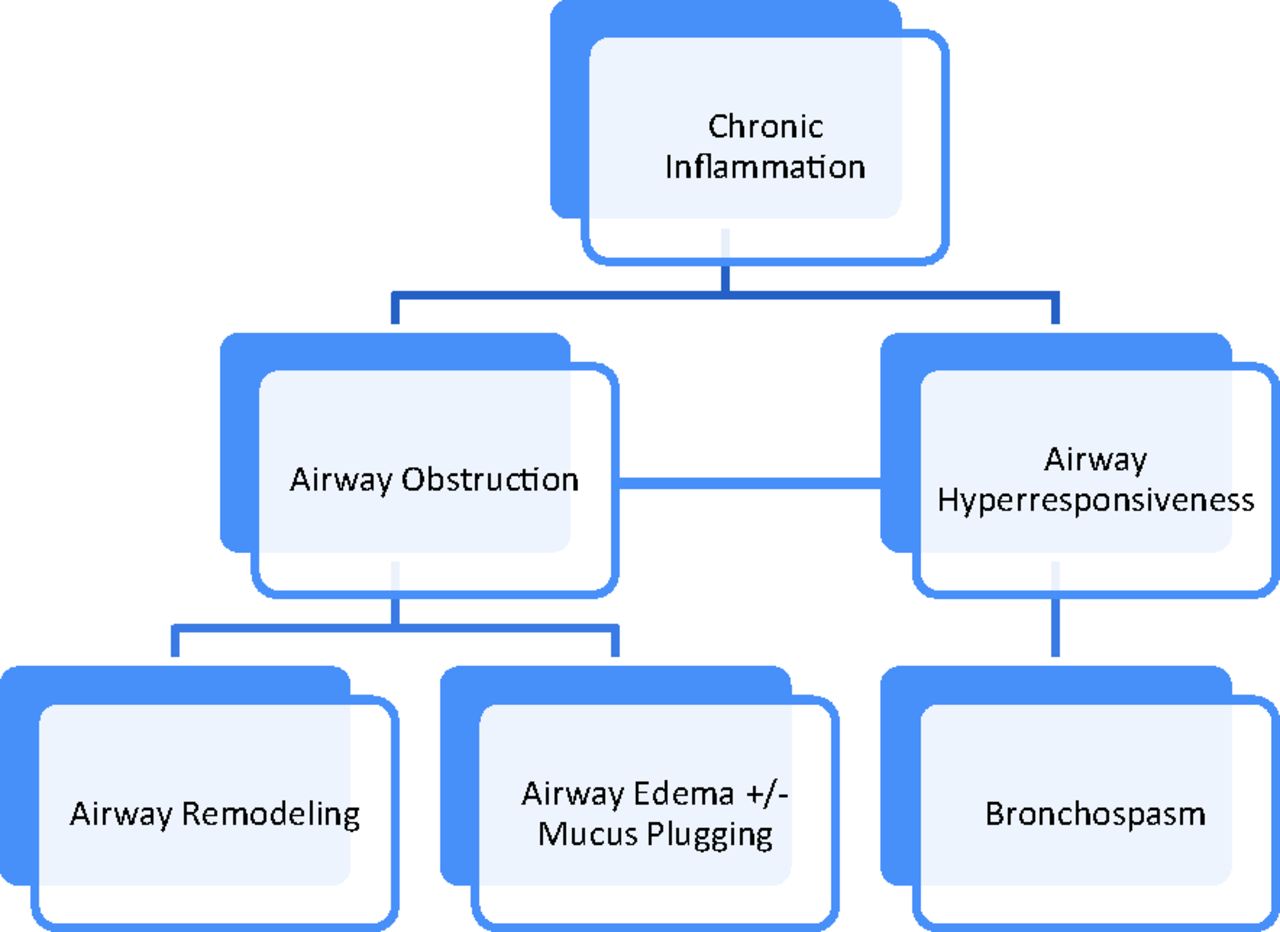
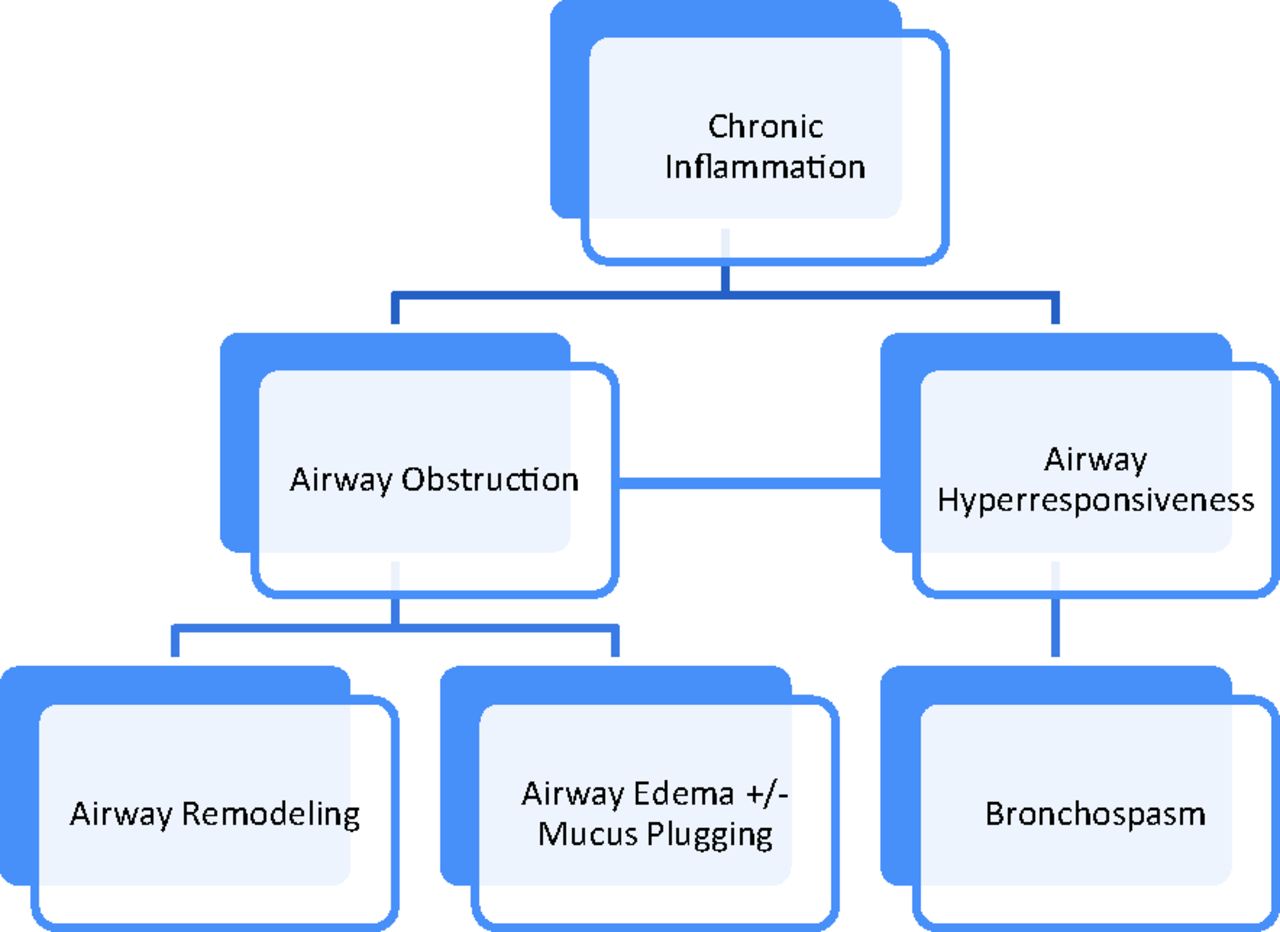
Clinical Recognition And Inflammatory Features Of The Overlap Syndrome: What Is It
The clinical recognition of both asthma and COPD requires assessment of symptoms and physiological abnormalities . Symptoms can indicate the presence of a disease process however, their sensitivity and specificity for asthma or COPD may be limited. At a physiological level, patients with overlap syndrome have evidence of incompletely reversible airflow obstruction that can be detected by a reduced postbronchodilator FEV1 . In addition, they have increased variability of airflow, which can be determined by increased bronchodilator responsiveness or BHR. The presence of airflow obstruction can confound the assessment of BHR in COPD. For recognition of the overlap syndrome, it may be preferable to use an indirect acting stimulus to assess BHR. Such agents do not directly cause airway smooth muscle contraction, and include hypertonic saline, adenosine and mannitol.
Informative data can be obtained from studies of discrete patient groups who have features of asthma and COPD. These groups include patients with asthma who smoke, those with asthma who develop incompletely reversible airflow obstruction and non-smokers who develop COPD. Smokers with asthma have features resembling COPD, since they are less responsive to corticosteroids and are less likely to have eosinophilic inflammation and more likely to have increased airway neutrophilia.
Also Check: What Is Asthma Characterized By
Epidemiology And Clinical Features
Without a standard definition or diagnostic system in place, the fact that population estimates of ACOS are highly variable comes as no surprise. Epidemiological studies have used definitions as disparate as the major-minor criteria system, self reported physician diagnoses, and combinations of spirometry results and symptom descriptions. Estimates of ACOS in the general population, using either self reported physician diagnoses or a combination of airflow obstruction on spirometry and symptom report, fall roughly between 2% and 3%.1240414243444546 In comparison, estimates of asthma and COPD in these same populations tend to be higher, around 5-17% for asthma and 2-12% for COPD. However, the prevalence of ACOS may vary according to geographic region, with estimates ranging anywhere from 0.61% in China to 3.7% in the United States.747 In cohorts of COPD patients specifically, the prevalence of ACOS ranges from 6% to 55%,6721464849505152535455565758 with pooled estimates from a meta-analysis suggesting a prevalence of just over 25%.5 In cohorts of asthma patients, the prevalence ranges from 10% to 31%.785559 In studies looking at patients with any airway obstruction , the prevalence ranges from 15% to 56%.1113606162 Moving forward, comparisons of prevalence across regions and time will ultimately require a standardised definition for ACOS. Nevertheless, no matter which definition is used, ACOS seems to account for a considerable portion of all airways diseases.
History Of Asthma Or Atopy Before Age 40years
Childhood asthma is common, affecting 10% of the population in industrialised countries. However, many children outgrow their asthma when they reach adulthood . Clinical features that are predictive of remission include lack of sensitisation and allergen exposure, higher baseline FEV1 and reduced airway hyperresponsiveness at the first assessment . Asthma can also develop in adulthood . Adult-onset asthma often occurs in non-atopic females with a history of rhinitis . It is often fraught with a large burden of symptoms and is associated with persistent airflow limitation and accelerated decline in lung function . It should be noted, however, that while both rhinitis and atopy are significant risk factors for asthma, elevating the risk of asthma by 1.67- and 3.90-fold, respectively , fewer than 50% of the adults with these features develop asthma . Interestingly, a recent study of ACOS suggested that COPD patients with a history of asthma may have different clinical features compared with COPD patients without a history of asthma including a significant BDR, higher eosinophil counts in the blood, and elevated total serum IgE concentrations .
Recommendation on history of asthma or atopy before age 40years
A history of childhood or adult-onset asthma should be a major criterion for ACOS. As the prevalence of COPD increases after age 40years, an age cutoff of 40years is reasonable to improve the accuracy of the diagnosis.
Don’t Miss: How To Rule Out Asthma
Paucigranulocytic Acoslong Acting Muscarinic Antagonists
For those ACOS patients without a distinct cellular inflammatory response, we return to bronchodilators, the stalwart of airways disease treatment. Ideally, for the patient with ACOS, bronchodilators should reduce ASM tone and dynamic hyperinflation. We have described the role of inhaled corticosteroid/LABA combinations in ACOS above here we discuss whether long acting muscarinic antagonists widely used in COPD have any benefit in asthma and, by extension, ACOS. Studies assessing the efficacy of LAMA therapy in asthma have largely evaluated tiotropium, an M1 and M3 receptor antagonist with a proven benefit in COPD. Several large, high quality randomised controlled trials have consistently shown improvements in FEV1 in patients with asthma, both in children and in adults, when tiotropium is added to inhaled corticosteroid and inhaled corticosteroid/LABA therapies.176177178179180181182 Several studies have also shown a reduction in exacerbation risk,179183 as well as asthma symptom control.179181182 Whether LAMA compounds other than tiotropium have similar positive effects is yet to be tested, but the clinical improvements observed in both COPD and asthma patients suggest that LAMA therapies may be an option for patients with ACOS.
Tobacco Smoking And Biomass Exposure
Recommendation on the environmental exposure for ACOS
Current or past cigarette smoking should be a major criterion for ACOS. However, there is uncertainty on the exact packyear cutoff that is appropriate for ACOS. Until more data are available, a reasonable cutoff is 10 packyears for smokers in countries where biomass exposure is not a major contributor to airflow limitation .
It should also be noted that in some parts of the world , indoor and outdoor pollution play a key pathogenic role in asthma and COPD in non-smokers or intermittent smokers. However, there is no universally accepted method to quantitate these exposures. Thus, in these jurisdictions, the committee recommends that this criterion may be fulfilled in non-smokers or smokers with < 10 packyears, who have equivalent biomass or outdoor air pollution exposure as deemed by their primary healthcare provider.
Also Check: Why Are Asthma And Eczema Related
Childhood: Risk Factors For Incomplete Lung Growth
Lung function in early adult life is a strong risk factor for the development of COPD. There is now evidence that poor lung function in infancy and childhood persists into adulthood, and that in utero events can modify airway function in early postnatal life. Stern et al studied lung function in infants soon after birth and found that poor airway function at that time was a risk factor for impaired adult lung function, suggesting that airway function throughout adult life may be determined during fetal development and the first few months of postnatal life. Maternal smoking adversely influences lung growth. In infancy there is an 1520% reduction in airflow in children born to mothers who smoked during pregnancy. In addition, maternal smoking is associated with impaired fetal growth, and intrauterine growth retardation is itself associated with impaired airway function in infancy and later life.
Many of the risk factors for incomplete lung growth in childhood are similar to the risk factors for accelerated loss of lung function in adults, namely tobacco smoke exposure, asthma, BHR and exacerbations or respiratory infections. Additional risk factors include low birth weight, gender , nutrition and ethnicity.
Asthma
Early life infections
Possibilities For Therapeutic Intervention
The myriad ways in which a particular person can potentially develop ACOS poses considerable challenges for treatment. The very heterogeneity of ACOS, the untoward by-product of a lack of consensus surrounding its pathophysiology and even its definition, implies that no single class of treatment is likely to help all patients. Importantly, we and others have advocated that the field move towards deeper phenotyping of these patients to guide treatment. In particular, as proposed by Barnes, three phenotypes of ACOS have been described that are important to establish before starting treatment: eosinophilic COPD , neutrophilic asthma , and paucigranulocytic ACOS.142 Needless to say, improved access to and standardisation of sputum cytology measurements is needed before such a strategy can be implemented. Even so, this framework provides a useful algorithm for targeting treatment of ACOS, one rooted in the presumed pathophysiology of the disease. In this section, we present the evidence for therapeutic options based on these three phenotypes, with the caveat that few trials have specifically investigated patients with ACOS. Extrapolations from asthma and COPD trials are thus also presented.
Recommended Reading: Can You Have An Asthma Attack In Your Sleep
How Might Copd Become Acos
The reverse scenario, in which a patient with COPD develops features of asthma, is admittedly less compelling. This would require the development of three important pathological traits of asthma in a patient with COPD: allergen sensitisation, airway hyper-responsiveness, and eosinophilic and type 2 mediated airway inflammation. Allergen sensitisation has been known to occur in COPD, particularly in older people,124 and upwards of 25-30% of COPD patients report allergic upper airway symptoms or show IgE sensitisation to perennial allergens.125 Among smokers, allergen sensitisation has also been associated with faster decline in lung function and, among COPD patients, with increased respiratory symptoms and COPD exacerbations.125126 Whether allergen sensitisation ultimately remodels the airway in the manner of asthma has yet to be demonstrated, however, and little research on this has been done. Similarly, airway hyper-responsiveness and eosinophilic/Th2 mediated inflammation also occur in COPD. However, for the former it is by no means certain whether the pathological process is the same as in asthma, and for the latter it is conceivable that similar inflammatory changes also occur in patients with asthma who develop ACOS. Below, we review the mechanisms by which these two features may emerge or worsen over the course of COPD.
Airway hyper-responsiveness and airway remodelling
Airway inflammation
